By Li Gai, Data Analyst at PCIC.
Putting patients at the center of care:
I had the privilege to participate in great conversations and connect with experts from diverse backgrounds who all care deeply about the High Needs High Cost population during the “Putting Care at the Center” conference in LA. It was so exciting to see practitioners, nurses, legislators, researchers, patients, social activists, and more come together and participate in the revolution of putting patients at the center instead of putting disease at the center of healthcare.
All the sessions I attended addressed different strategies for personalizing healthcare to put the patient at the center, but one message stood out and stuck in my head: Get patients involved in the conversation and get their voices heard. The message was appealing to me because it so closely aligns with the Value-based Care Coordination model we are implementing at PCIC. I also realized that there is so much more we could do to help revolutionize the way care is provided.
So, what is our Value-based Care Coordination model? And what role can technology play in implementing it?
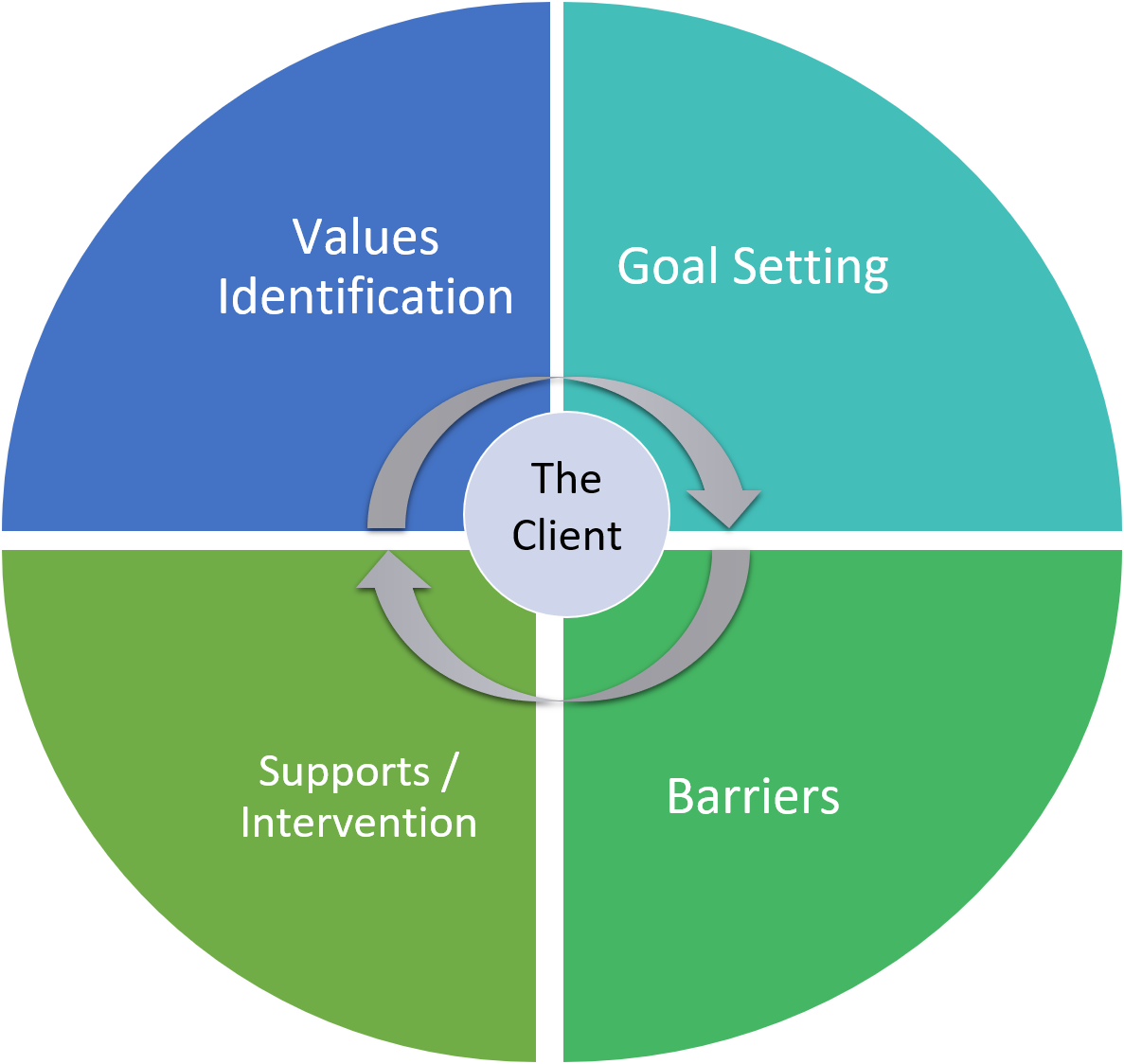
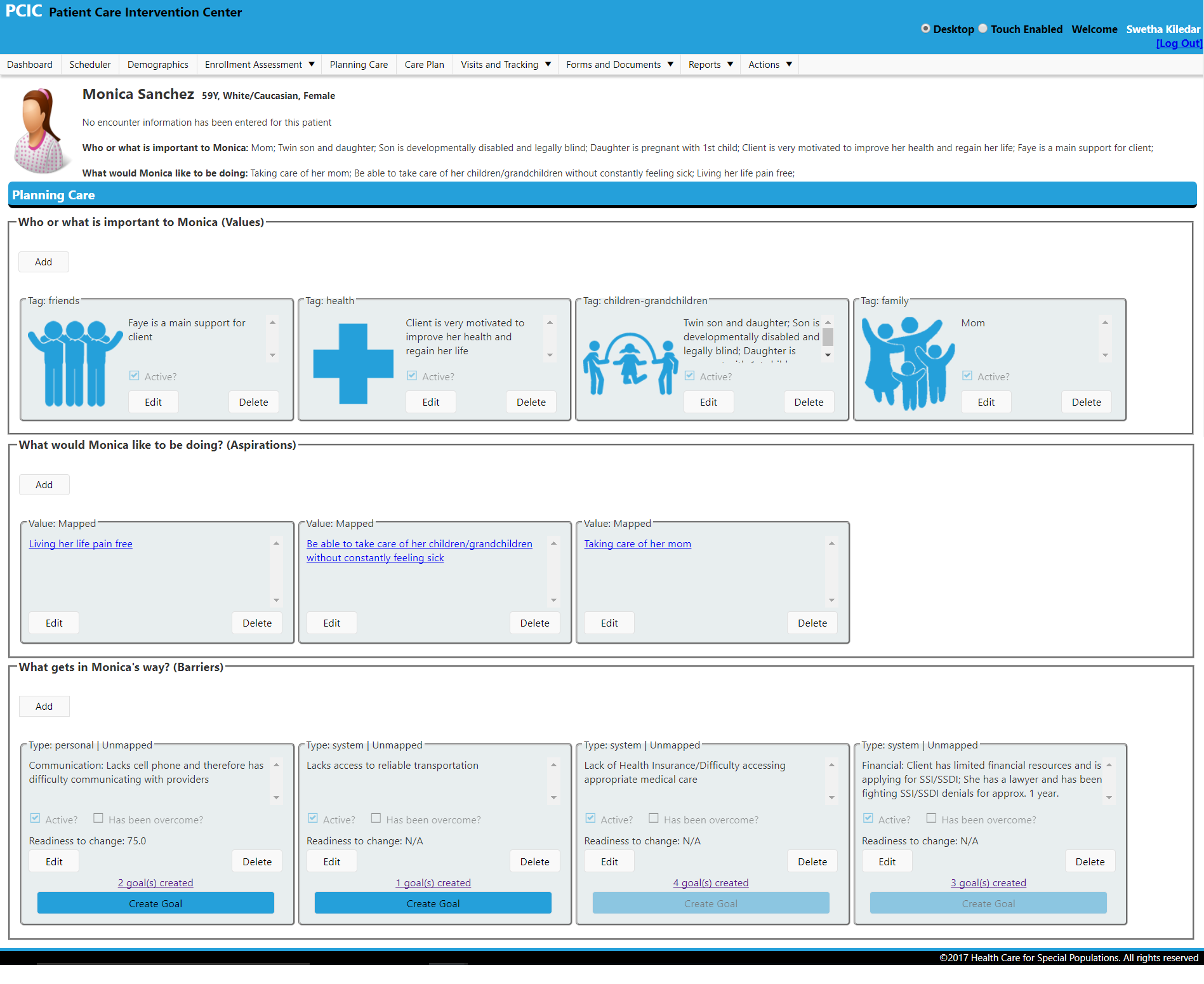
At PCIC, we aim to develop a data-driven, client-centered, value-based coordinated care model for Electronic Health Record software to integrate care and increase communication across agencies. With the help of StreetEMR, our case management, analysis and tracking software, we assess each client’s social determinants of health during visits. The areas we are currently assessing are: housing, economic stability, food and nutrition, healthcare and community support. The assessment opens up a window for care coordinators to get to know the client as well as for the client to disclose the barriers they face that might be stopping them from obtaining a healthier life. The guided tool has already been built into StreetEMR to help the team document insights about patients, while exploring with the client which things they value most in life, what their short term and long term goals are, and what gets in the way of them achieving these aspirations.
We are working on implementing self-learning algorithms to help automatically identify gaps in client care and recommend resources with which we can connect our clients. Using the value based model, we will be able to motivate our clients to work towards negotiated goals that matter most to them. This increases patient buy-in for interventions, strengthens trust in the patient-provider relationship, all the while improving health outcomes.
What’s next:
We are always looking for ways to improve the way we communicate with our clients, and one of the items high on the list is natural language processing (NLP). It can help care coordination team understand and identify values, goals and barriers while having a conversation with the patient. It can also assist in answering difficult questionnaires such as the Adverse Childhood Experiences survey. Another item we definitely need to work on is to improve UI design to lead the conversation of discovering “what happened” instead of “what is wrong.“ For example, if a client is a frequent heroin user, aside from documenting the doses and frequency of drug usage, the system should also be designed to naturally lead the coordinators to ask “why” the client is using the drug and “what” they are trying to cope with. If they are trying to self-medicate for anxiety, providing appropriate anti-anxiety medication might be as important to their recovery as stopping their heroin use. The list of to-do items will keep growing as we practice our model and learn from our successes and failures. We are always stronger as a group, and our goal at PCIC is to identify and partner with likeminded organizations to deliver better solution for our clients and community. “If you cannot get out of it, get more into it,” said one of the inspiring keynote speakers from the conference, and I think we are ready to get all into it.